Shoulder Impingement
One of the more common injuries I see at Range of Motion Physical Therapy is shoulder impingement pain. Our shoulders are made up of several joints combined with tendons and muscles that allow a great range of motion of the arm. The shoulder is vulnerable to many different problems, I will focus on the more common source of pain and injury, the rotator cuff and resulting in impingement.
The rotator cuff keeps the head of the humerus in the shoulder socket. There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). This bursa allows the rotator cuff tendons to glide freely when you move your arm.
Types of complications:

Tendinitis. The rotator cuff tendons can be irritated or damaged.
Bursitis. The bursa can become inflamed and swell with more fluid causing pain.
Impingement. When you raise your arm to shoulder height, the space between the acromion and rotator cuff narrows. The acromion can rub against (or “impinge” on) the tendon and the bursa, causing irritation and pain.
Rotator cuff injuries are common in both athletes and middle-aged people, athletes who participate in overhead sports such as swimming, baseball, or tennis are particularly vulnerable. Those who do repetitive lifting or overhead activities using the arm, such as paper hanging, construction, or painting are also susceptible from over use issues.
Symptoms:
Minor pain that is present both with activity and at rest
Pain radiating from the front of the shoulder to the side of the arm
Sudden pain with lifting and reaching movements
As the problem progresses, the symptoms can worsen:
Pain at night lying on shoulder
Loss of strength and motion in the shoulder
Shoulder pain reaching arm behind the back
I would always advise people seek help for an injury that persists for more than 10 days.
Treatment:
In most cases, initial treatment is conservative involving rest, ice and gradual return to function. A physical therapy treatment will include postural assessment and orthopedic test to identify any postural/muscle imbalances in the shoulder and the cause of the impingement. Treatment will involve hands on soft tissue work, strengthening and stretching targeted muscles, to improve movement patterns and prevent the impingement and pain. As your pain is improving, a shoulder strengthening program for the rotator cuff muscles will be initiatated
How I Best Serve My Clients!
How I Best Serve My Clients at Range of Motion Physical Therapy.
As it is the start of a new year I like to ask myself “What do I do differently now than 1 year ago?” If the answer to that is nothing, I feel I am doing a disservice to myself and my clients. When I asked myself that question recently, I am happy to say there were a number of areas I have changed or up skilled in how I treat my clients, below are a few examples: My exercise selection for client rehabilitation, regardless of whether I am treating a sports injury or a mobility issue. I have looked to select the most effective and suitable exercise for the clients injury and capability. I try to avoid loading to many exercises on clients and rather look at the number of reps and sets being done, to ensure the exercises are making a positive impact on the client’s injury. My treatment protocol and technique selection, in the past couple of years I have attended a number of courses on joint manipulations, ranging from high velocity Grade 5 manipulations to low amplitude manipulations. By continually learning and doing courses, I have more flexibility to choose from soft tissue work, muscle release, manipulations or a combination of all when treating clients. This lets me tailor my treatments when working with a wide range of the population. Serving my clients better, I am happy to say I regularly research different treatment techniques and the best exercises for certain injuries. I keep myself up to date on new advances in various areas by following professional blogs, reading books and articles from different fields, such as strength & conditioning and personal training. As a Physical Therapist I work with a wide range of clients, resulting in a wide range of issues such as sports injuries, post surgical rehabilitation, acute injuries and repetitive strain issues from active daily living. With this in mind it is important to self assess my treatments and skills and look to stay in touch with new research, learning and offer my clients the best possible treatment I can provide.
Whiplash and Neck Pain
What is Whiplash?
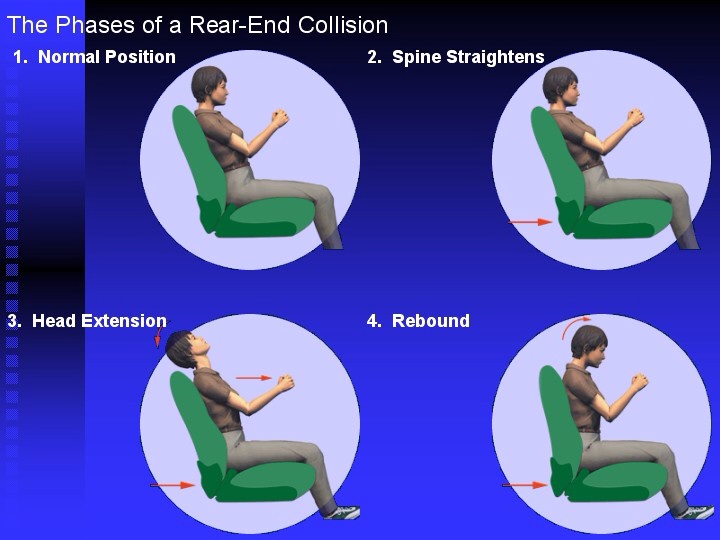
Whiplash is a neck injury that can occur during a rear end car accident or during contact sports such as rugby. Whiplash and neck pain occurs when your head suddenly moves backward and then forward. These extreme motions push your neck muscles and ligaments beyond their normal range of motion.
Whiplash injuries can be mild or severe. Treatment typically begins with over-the-counter pain relievers and ice applied to the painful neck muscles. If pain persists, prescription medications and physical therapy may be helpful. Most people recover from whiplash in just a few weeks, but some people may develop chronic pain after a whiplash injury.
What Are the Symptoms of Whiplash?
Symptoms of whiplash may be delayed for 24 hours or more after the initial trauma. However, people who experience whiplash may develop one or more of the following symptoms, usually within the first few days after the injury.
Neck pain and stiffness
Headaches
Pain in the shoulder or between the shoulder blades
Low back pain
Pain or numbness in the arm and/or hand
Dizziness
Ringing in the ears or blurred vision
Difficulty concentrating or remembering
Irritability, sleep disturbances, fatigue
In most cases, whiplash injuries are classified as soft tissue injuries, with structures such as the disks, muscles and ligaments being damaged. These structures cannot be seen on standard X-rays, specialised imaging tests, such as CT scans or (MRI) may be required to diagnose whiplash or rule out any other possible causes. However should you have any of the above symptoms following an accident, seek medical help.
How Is Whiplash Treated?
Many people with whiplash pain find it helpful to use ice or heat on their necks and upper backs. In general, ice should be used early in the recovery period, to reduce inflammation, while heat is especially helpful to relax muscles before range of motion exercises.
If over-the-counter pain medications and self-care treatments at home aren’t enough, your doctor may suggest physical therapy. Physical therapy interventions are the mainstay of treatment for whiplash. Therapy treatments may include:
Ice
Heat
Manual therapies, including myofascial release
Stretch & Strengthening exercises
Rehab exercises can help to minimise symptoms, help protect your neck in the future and speed up recovery. Immobilising the neck for long periods of time can lead to decreased muscle bulk, strength and impair recovery.
Restricted Knee Movement and Knee Pain Walking
Restricted Knee Movement and Knee Pain Walking
An elderly lady (83 yr old) contacted me 3 weeks ago looking to make an appointment, she told me she found me @ www.romphysicaltherapy.ie when she googled Physical Therapy Lucan, she is 83 yr old, cool super granny.
Her Chiropractor had suggested she get some physical therapy on the back of her knee due to posterior knee pain and restriction. She had been attending her chiropractor for a number of years having manipulations carried out every 3-4 weeks, it has gotten to the stage were she would only get a couple of days relief following the manipulations on her spine, pelvis and occasionally on her knee.
On her first appointment she reported intermittent knee pain at the back of the knee at 5/10, pain walking, going down the stairs and moving from sitting to standing position, she has been going up and down the stairs sideways, one step at a time for a number of years.
Her knee is restricted to 160 degrees of extension and 90 degrees of flexion, with a hard end feel, this range may never improve due to OA. She also had hypertonic gastroc, quad and her popliteaus muscle was tender on palpation.
The 1st appointment involved the assessment and some simple soft tissue work (STW) to calf, hamstring, quads and popliteaus, hip & knee mobs. Home exercise was simple repeated knee extension exercise.
2nd appointment she reported the knee has felt loser, less pain walking 3/10 and relief lasted a few days, on examination gastro was still hypertonic and pain on palpation, popliteaus muscle had released significantly. Home exercises involved more hip strengthening exercise: Single Leg Raises, Clam, Abduction and Quad Sets. She was due to have an app with her chiropractor before her next appointment.
3rd appointment she reported very little pain in the back of the knee, she was now walking up and down the stairs correctly with slight pain, she never thought she would be able to do it. At her chiropractor visit the chiropractor said the lumber spine and sacro illiac joint was no longer misaligned and she did not carry out a manipulation on this region for the first time in years.
I have added some simple step up/down exercises to assist with her single leg strength, to facilitate her going up and down the stairs. The client commented she should have started exercises a long time ago but felt they would make her worse…..years of manipulations with little improvement and lessening relief, 3 weeks of simple isolated strengthening exercises and she is now climbing stairs and walking pain free….go figure!!!
She is due back in 10 days so hopefully she is flying up and down the stairs. Forgot to mention that she also has a stair lift at home which she refuses to use!!!
Range of Motion Physical Therapy Gift Vouchers
Range of Motion Physical Therapy Gift Vouchers
Treat someone special to a Christmas Gift Voucher from Range of Motion Physical Theapy
A great Christmas present idea for someone in your life that does a lot of training or enjoys a good deep tissue or sports massage.
Gift Vouchers now available for Christmas and special occasions, contact me should you wish to place an order!!
Plantar Fasciitis:
At Range of Motion Physical Therapy Lucan, we see a lot of clients with plantar fasciitis, below is an article to give you an overview and some good exercises to help prevent and treat plantar fasciitis.
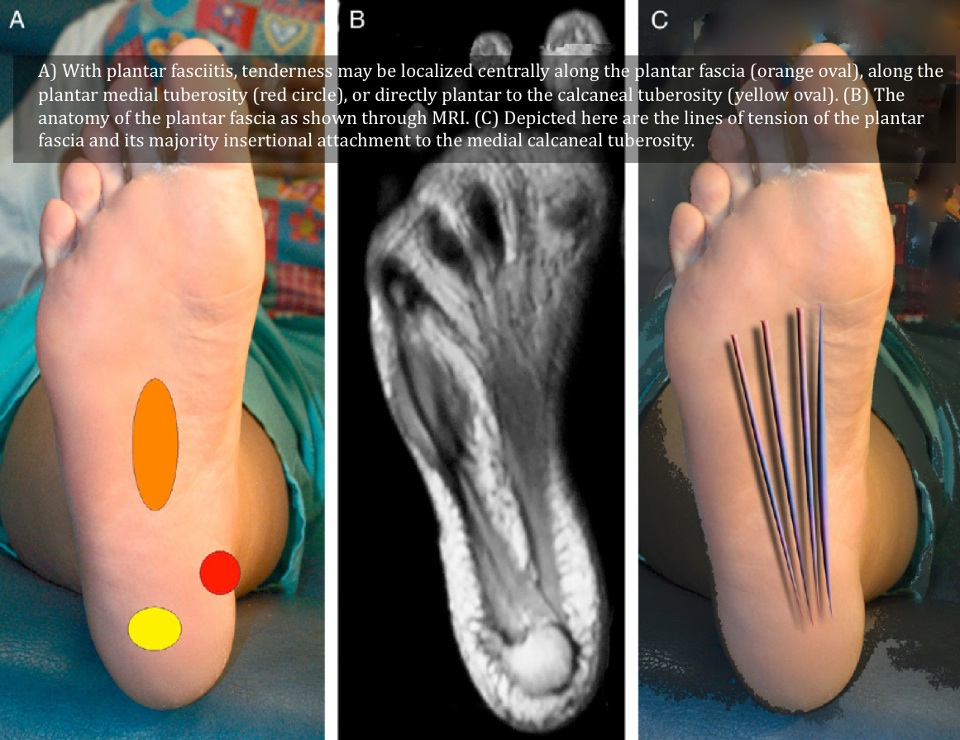
The plantar fascia is a ligament (attaches bone to bone) that supports the arch of the foot. Plantar fasciitis is a degenerative condition of the fascia which is probably caused by repetitive microtrauma and occurs at its proximal attachment. Plantar fasciitis affects mainly middle aged or older people and those who walk a lot and/or have an increased body weight are more at risk.
Reduced range of ankle dorsiflexion, calf- and hamstring tightness are associated with plantar fasciitis.
Differential diagnosis: Achilles tendinopathy, subtalar arthritis, S1 nerve root impingement, fat pad contusion, calcaneal bone bruise or stress fracture.
Symptoms:
- Pain and tenderness of the bottom (sole) of the foot.
- Pain weight-bearing on the involved foot, especially the first steps after awakening from sleep.
- Pain is burning, often sharp, and can be severe.
- The symptoms may come on gradually or appear following an athletic activity.
Treatment options:
- Foot Strenghtening Exercises
- Footwear modifications to reduce pronation and thereby unload the plantar fascia.
- Stretching techniques (night splints)
- Extracorporeal shock wave
- Cortisone injections
- Surgery
- Weight loss
Some interesting Foot Arch Strengthening Exercises to try!!!
Arch Strengthening Exercise:
If you are experiencing any of the symptoms above contact us for an assessment and treatment on how to resolve this issue.
British Medical Journal 345 (2012) e6603. All rights reserved to BMJ Publishing Group Ltd.
Resolute Pilates & Fitness
We have set up a nice working relationship with Denise @ www.resolute.ie pilates studios. Check out their website for more information on classes etc… Denise comes highly recommended!
Resolute is the first & only Studio in Clondalkin specifically catering for Pilates and Exercise Rehabilitation. Based in Unit 19 Bawnogue Enterprise Centre, it is their mission at RESOLUTE to provide Pilates and Exercise Courses with an emphasis on how each person is different and therefore needs a more Personalized and Individual approach to exercise.
Achilles Tendonitis Prevention & Treatment Programme
Following on from a previous Service Your Body Physical Therapy post on Achilles Tendonitis I have included a programme of exercises to help prevent and treat Achilles Tendonitis.
These exercise are taken from Sports Injury Bulletin and are based on evidence based research from clinical experts (Raphael Brandon & Harvey Wallmann)
PREVENTION PROGRAMME
To look at the prevention of achilles injuries we must first understand that there is a relationship that the achilles tendon has with both the calf muscles (gastrocnemius and soleus).
EMG data shows that the calf muscles are most active just before and just after foot strike and then their key function is to control dorsiflexion and pronation. It is in turn these two actions (performed to a lesser or greater degree depending on varying factors in the athletes physiology) due to the force and stretching that cause damage to the achilles tendon.
As well as looking at dorsiflexion and pronation we must also look at the kinetic chain, and if the imbalance is coming from the foot up or the pelvic girdle down.
The four key exercises below mimic the kinetic chain of events within the calf muscles and achilles when you run. (Something that interestingly, some experts believe that calf raises do not)
Exercise 1. Eccentric Knee Squat & Single leg Squat
Exercise 2. Balance and Eccentric Reach with Toes
Exercise 3. Balance and Eccentric Reach with Knee
Exercise 4. Dynamic Achilles Stretch
Follow link to a video of how to do above exercises poor quality!!
The exercises should be progressive, make sure to start with exercises performed in a sagittal direction and progressing onto exercises performed in a transverse direction (right to left that are more dynamic).
STRENGTHENING PROGRAMME
Other factors that must be taken into consideration are incorrect running shoes, hard or uneven running surfaces and unrealistic increases of mileage/training intensity (work on a guideline of 5-10% increase in mileage per week).
The achilles injuries can also be caused by lack of flexibility and strength in the calf muscles, this will become most apparent when running up hill.
It is important to create a training program to increase the eccentric strength of the calf (when a muscle lengthens as it contracts) using progressively faster speeds of movement to increase the forces that the calf can handle.
The rehabilitation exercises should take place after 1 to 2 weeks of rest once pain and inflammation have gone down.
The program below should be performed everyday:
1. Warm-Up – 5-10 minutes of CV – non weight bearing e.g cycling etc.
2. Stretching – For both gastrocnemius and soleus, perform 3 x 30secs stretches on both sides.
3. Eccentric Programme –
Level 1 – Perform a straight legged heel raise with uninjured leg, then place the ball of the injured leg down and lower slowly with both legs until the heels reach the floor. Progress as follows:
Drop time: 4secs 3×10 reps. with 30 seconds rest.
Drop time: 2seconds 3 x10 reps. with 30 seconds rest.
Drop time: 1secs 3 x10 reps. with 30 seconds rest.
Repeat from the beginning (as above) performing a bent-legged heel raise – knee should be bent 20-30degrees.
Level 2 – Perform heel raises with both legs for lowering and raising phases. 3X10reps with 30 seconds rest. Progress as in level 1.
Level 3 – Perform heel raises with the uninjured leg on the raise phase and with the injured leg on the lower phase. 3X10reps with 30 seconds rest. Progress as in level 1.
Level 4 – Perform heel raises with both legs during the raising phase with only injured leg during the lowing phase. 3X10reps with 30 seconds rest.
Level 5 – Perform heel raise lowering and raising with only the injured side. 3X10reps with 30 seconds rest. Progress as in level 1.
4. Stretching – Follow point 2.
Please contact us at Range of Motion Physical Therapy if you need any additional information or advise on this or other injuries.
- See more at: http://www.romphysicaltherapy.ie/index.php/achilles-tendonitis-prevention-treatment-programme/#sthash.G3CzYs4U.dpuf
Thoracic Pain
At Range of Motion Physical Therapy, Lucan I had a client who works as a tiler report with thoracic pain and shoulder pain, he also had pain traveling down his left arm to his elbow. He could not sleep with the pain down the arm and had to keep moving to find a position of ease, he was also restricted in neck extension and rotation to the involved side.
Treatment 1: following assessment it was evident T4 L facet was jarred causing shoulder and neck muscle tightness with Radial nerve referral to his elbow. My treatment involved soft tissue work to his neck, shoulder and (Massage with Movement) MWM mobs to thoracic and cervical spine. I completed the treatment with Dry Needling to the thoracic region. Two days later the client reported a small improvement but following a days work the symptoms came back worse than ever, so much so he had to take a day off work.
Treatment 2: The clients referral had moved past his elbow to his thumb and index finger. Again I carried out some more thoracic and cervical MWM mobs, I followed up with some additional soft tissue work to neck, shoulder and upper arm. My treatment also included some nerve flossing techniques to release the radial nerve. As home exercises I showed the client how to carry out some self Thoracic mobs and Radial nerve flossing, he was instructed to them hourly or as often as possible.
I contacted the client the following day and he reported he slept for 14 hours, without waking once and had full movement of his neck with just a slight referral into his tricep muscle.
Treatment 3 & 4 comprised of additional STW to neck and shoulders with mobilisations to his cervical and thoracic region, while continuing the nerve flossing techniques.
Two weeks following on from his last appointment the client has reported that he is pain free with full range of motion of neck and shoulder with no referral.
- See more at: http://www.romphysicaltherapy.ie/index.php/thoracic-pain/#sthash.iuaz41Tk.dpuf
Swimmers Shoulder
Being a keen swimmer myself I suffer a little with tight shoulders due to my training and the hands on treatments I do at Range of Motion Physical Therapy, Lucan. Swimmers shoulder is the term used to describe the problem of shoulder pain in a swimmer. Below is an overview of the injury but it is more of an issue with rotator cuff tendonitis and shoulder pain impingement which we can all suffer from due to posture and our work.
Swimming is an unusual sport in that the shoulders and upper extremities are used for locomotion, while at the same time requiring above average shoulder flexibility and range of motion (ROM) for maximal efficiency. This is often associated with an undesirable increase in joint laxity. Furthermore, it is performed in a fluid medium, which offers more resistance to movement than air. This combination of unnatural demands can lead to a spectrum of overuse injuries seen in the swimmer’s shoulder, the most common of which is rotator cuff tendinitis.
Rotator Cuff: the key muscle group of the shoulder is the rotator cuff, made up of the subscapularis, supraspinatus, infraspinatus, and teres minor. The primary role of the rotator cuff is to function as the dynamic and functional stabiliser of the glenohumeral joint. These muscles and their tendons can be overused and injured in shoulder dominant activities such as swimming, with the most commonly injured portion of the cuff being the supraspinatus.
Rotator cuff tendinitis, or impingement syndrome, may be due to:
- Keeping the arm in the same position for long periods of time, such as doing computer work or hairstyling
- Sleeping on the same arm each night
- Playing sports requiring the arm to be moved over the head repeatedly as in tennis, swimming, and lifting weights over the head
- Working with the arm overhead for many hours or days (such as in painting and carpentry)
- Poor control or coordination of your shoulder and shoulder blade muscles
- Poor posture over many years and the usual fraying of the tendons that occurs with age may also lead to rotator cuff tendinitis.
Symptoms:
- Pain is more likely in the front of the shoulder and may radiate to the side of the arm. However, this pain always stops before the elbow. If the pain travels beyond the arm to the elbow and hand, this may indicate a pinched nerve.
- There may also be pain with lowering the shoulder from a raised position.
- At first, this pain may be mild and occur only with certain movements of the arm. Over time, pain may be present at rest or at night, especially when lying on the affected shoulder.
- You may have weakness and loss of motion when raising the arm above your head. Your shoulder can feel stiff with lifting or movement. It may become more difficult to place the arm behind your back.
Treatment initially involves resting the shoulder and avoiding activities that cause pain. It may involve:
- Ice packs applied 20 minutes at a time, 3 – 4 times a day to the shoulder
- Avoiding or reducing activities that cause or worsen your symptoms to worsen
- You should start physical therapy to learn exercises to stretch and strengthen the muscles of your rotator cuff.
- With rest and exercise, symptoms often improve or go away. However, this may take weeks or months to occur.
For more information about managing your symptoms at home and returning to sports or other activities, contact me at Range of Motion Physical Therapy, Lucan.